Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Nose Injuries
Nose injuries often occur during play, sports, accidents, fights, and falls. Pain, swelling, and bruising are common, even with minor injuries. Home treatment can usually help relieve your symptoms.
It may be hard to tell if your nose is broken. Swelling can make your nose look crooked even if it isn't broken. When the swelling goes down after a few days, it's easier to tell if your nose is really crooked. Most doctors prefer to check an injured nose soon after the swelling has gone down. Sometimes testing may be needed, such as an X-ray or CT scan of the head, if the doctor thinks you might have other facial injuries or fractures.
Seriousness of a nose injury
Whether or not your nose is broken, a nose injury is more serious when:
- You have a nosebleed that you can't stop.
- The skin of your nose is cut or punctured, especially if you think your nose may be broken. This increases your risk of infection.
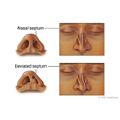
- A blood clot forms in the tissue that separates the nostrils (septum). This can create a hole (perforation) in the septum. Or it can cause the bridge of the nose to collapse (saddle nose deformity).
- You think the injury may have been caused by abuse. Physical abuse often causes bruises, burns, fractures, head injuries, and other injuries. If you suspect abuse, seek help. You can call a local child or adult protective services agency, the police, a spiritual advisor, or a health professional such as a doctor, nurse, or counselor.
- You have drainage that won't stop from one or both nostrils. This may be caused by cerebrospinal fluid (CSF) draining from the brain into the nose (CSF rhinorrhea). It can occur after a head injury or after surgery on the nose or ears. There is a chance that you may get a CSF infection, such as meningitis. It can affect the nervous system and be life-threatening.
Complications of a broken nose
Most broken noses heal without problems. When problems occur, they can include:
- A change in the size or shape of the nose, or a crooked or bent nose. Multiple nose injuries, especially during childhood, increase the risk of damage to the tissues and structures in the nose. This can cause long-term problems.
- Trouble breathing or a stuffy nose.
- An infection of the nose, sinuses, or bones in the face.
- A problem with the tissue that separates the nostrils (deviated nasal septum).
- A hole (perforation) in the septum.
- Severe infection, such as meningitis or a brain abscess, or other CSF infection.
Treatment
Treatment of a simple fracture, when the bone is still in place, usually includes pain medicine and nasal decongestants. You may or may not need a nasal splint.
If your nose is broken and out of place, it may need to be set. Most doctors like to wait for any swelling to go down before they set a broken nose. Most swelling goes down after 2 or 3 days, but it may take as long as 7 to 14 days. After the nose is set, nasal packing may be inserted. You may also get a splint. You may get antibiotics to help prevent infection if packing is used. Your doctor may want to recheck your nose and remove the packing in 2 to 5 days.
When you have a nose injury, it's important to look for other injuries to the head, face, and neck. These may include a broken cheekbone, an eye injury, an injury to the mouth or teeth, or a cervical spine injury.
Check Your Symptoms
The medical assessment of symptoms is based on the body parts you have.
- If you are transgender or nonbinary, choose the sex that matches the body parts (such as ovaries, testes, prostate, breasts, penis, or vagina) you now have in the area where you are having symptoms.
- If your symptoms aren’t related to those organs, you can choose the gender you identify with.
- If you have some organs of both sexes, you may need to go through this triage tool twice (once as "male" and once as "female"). This will make sure that the tool asks the right questions for you.
Many things can affect how your body responds to a symptom and what kind of care you may need. These include:
- Your age. Babies and older adults tend to get sicker quicker.
- Your overall health. If you have a condition such as diabetes, HIV, cancer, or heart disease, you may need to pay closer attention to certain symptoms and seek care sooner.
- Medicines you take. Certain medicines, such as blood thinners (anticoagulants), medicines that suppress the immune system like steroids or chemotherapy, herbal remedies, or supplements can cause symptoms or make them worse.
- Recent health events, such as surgery or injury. These kinds of events can cause symptoms afterwards or make them more serious.
- Your health habits and lifestyle, such as eating and exercise habits, smoking, alcohol or drug use, sexual history, and travel.
Try Home Treatment
You have answered all the questions. Based on your answers, you may be able to take care of this problem at home.
- Try home treatment to relieve the symptoms.
- Call your doctor if symptoms get worse or you have any concerns (for example, if symptoms are not getting better as you would expect). You may need care sooner.
Pain in adults and older children
- Severe pain (8 to 10): The pain is so bad that you can't stand it for more than a few hours, can't sleep, and can't do anything else except focus on the pain.
- Moderate pain (5 to 7): The pain is bad enough to disrupt your normal activities and your sleep, but you can tolerate it for hours or days. Moderate can also mean pain that comes and goes even if it's severe when it's there.
- Mild pain (1 to 4): You notice the pain, but it is not bad enough to disrupt your sleep or activities.
Pain in children under 3 years
It can be hard to tell how much pain a baby or toddler is in.
- Severe pain (8 to 10): The pain is so bad that the baby cannot sleep, cannot get comfortable, and cries constantly no matter what you do. The baby may kick, make fists, or grimace.
- Moderate pain (5 to 7): The baby is very fussy, clings to you a lot, and may have trouble sleeping but responds when you try to comfort him or her.
- Mild pain (1 to 4): The baby is a little fussy and clings to you a little but responds when you try to comfort him or her.
To stop a nosebleed:
- Gently blow your nose to clear any clots.
- Sit up straight, and tip your head slightly forward. (Do not tilt your head back. This may cause blood to run down your throat and make you vomit.)
- Pinch the front, soft part of your nose shut with your thumb and index finger for at least 15 minutes.
- After 15 minutes, check to see if your nose is still bleeding. If it is, pinch it shut for 10 to 15 more minutes. Most nosebleeds will stop after 10 to 20 minutes of pressure.
Symptoms of infection in the nose may include:
- Increased pain, swelling, warmth, or redness around the nose.
- Pus or smelly drainage from the nose.
- Fever.
Certain health conditions and medicines weaken the immune system's ability to fight off infection and illness. Some examples in adults are:
- Diseases such as diabetes, cancer, heart disease, and HIV/AIDS.
- Long-term alcohol and drug problems.
- Steroid medicines, which may be used to treat a variety of conditions.
- Chemotherapy and radiation therapy for cancer.
- Other medicines used to treat autoimmune disease.
- Medicines taken after organ transplant.
- Not having a spleen.
A nosebleed is severe if:
- You have moderate to large amounts of blood even after you have pinched the nose shut for 10 minutes.
- Your nose is still bleeding even after 15 full minutes of direct pressure.
A nosebleed is moderate if:
- You have some bleeding, but direct pressure stops it within 15 minutes.
- The nose bleeds small amounts of blood more than 3 times in 24 hours.
A nosebleed is mild if:
- You have a little bleeding, but direct pressure stops it within 10 minutes.
- The nose bleeds no more than 3 times in 24 hours, and each time the bleeding is mild.
Usually found in dirt and soil, tetanus bacteria typically enter the body through a wound. Wounds may include a bite, a cut, a puncture, a burn, a scrape, insect bites, or any injury that may cause broken skin. Tetanus can also happen with other infections, like dental infections. It can happen during a surgery or pregnancy and delivery.
A wound can be so small, you may not notice you have one. Or a skin blister could break and become an open wound. If there is any delay in finding or cleaning a wound, there is an increased risk for skin infection and a chance for tetanus to get in the wound. A tetanus infection can start 3 to 21 days after the bacteria enter the wound. Be especially careful about wounds on your fingers and toes.
Many people may not know when they got their last tetanus shot. So it's a good idea to call your doctor to see if you need one.
Make sure to stay up to date on your tetanus shots. A tetanus shot is recommended:
- For a dirty wound that has things like dirt, saliva, or feces in it, if you haven't had a tetanus shot in the past 5 years.
- For a clean wound, if you haven't had a tetanus shot in the past 10 years.
Symptoms of a skull fracture may include:
- Clear or bloody fluid draining from the ears or nose.
- Bruising under the eyes or behind the ears.
- Drooping of the face.
- A dent anywhere on the head.
The symptoms of a skull fracture may appear at the time of the injury or hours or days later.
Symptoms of difficulty breathing can range from mild to severe. For example:
- You may feel a little out of breath but still be able to talk (mild difficulty breathing), or you may be so out of breath that you cannot talk at all (severe difficulty breathing).
- It may be getting hard to breathe with activity (mild difficulty breathing), or you may have to work very hard to breathe even when you're at rest (severe difficulty breathing).
Severe trouble breathing means:
- You cannot talk at all.
- You have to work very hard to breathe.
- You feel like you can't get enough air.
- You do not feel alert or cannot think clearly.
Moderate trouble breathing means:
- It's hard to talk in full sentences.
- It's hard to breathe with activity.
Mild trouble breathing means:
- You feel a little out of breath but can still talk.
- It's becoming hard to breathe with activity.
Severe trouble breathing means:
- The child cannot eat or talk because he or she is breathing so hard.
- The child's nostrils are flaring and the belly is moving in and out with every breath.
- The child seems to be tiring out.
- The child seems very sleepy or confused.
Moderate trouble breathing means:
- The child is breathing a lot faster than usual.
- The child has to take breaks from eating or talking to breathe.
- The nostrils flare or the belly moves in and out at times when the child breathes.
Mild trouble breathing means:
- The child is breathing a little faster than usual.
- The child seems a little out of breath but can still eat or talk.
Shock is a life-threatening condition that may quickly occur after a sudden illness or injury.
Adults and older children often have several symptoms of shock. These include:
- Passing out (losing consciousness).
- Feeling very dizzy or lightheaded, like you may pass out.
- Feeling very weak or having trouble standing.
- Not feeling alert or able to think clearly. You may be confused, restless, fearful, or unable to respond to questions.
Shock is a life-threatening condition that may occur quickly after a sudden illness or injury.
Babies and young children often have several symptoms of shock. These include:
- Passing out (losing consciousness).
- Being very sleepy or hard to wake up.
- Not responding when being touched or talked to.
- Breathing much faster than usual.
- Acting confused. The child may not know where he or she is.
Seek Care Now
Based on your answers, you may need care right away. The problem is likely to get worse without medical care.
- Call your doctor now to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don't have one, seek care in the next hour.
- You do not need to call an ambulance unless:
- You cannot travel safely either by driving yourself or by having someone else drive you.
- You are in an area where heavy traffic or other problems may slow you down.
Seek Care Today
Based on your answers, you may need care soon. The problem probably will not get better without medical care.
- Call your doctor or telehealth provider today to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or telehealth provider or you don't have one, seek care today.
- If it is evening, watch the symptoms and seek care in the morning.
- If the symptoms get worse, seek care sooner.
What are your options for medical care?
Today your options for where to get your medical care are greater than ever before. You may not even have to leave your home to get the care you want and need. You can choose based on what your health problem is and what works best for you.
- Telehealth is a video call with a health care provider. It can be a convenient way to get medical advice or treatment. Some insurers provide access to telehealth that may be available 24 hours a day. Telehealth for less serious problems may cost less and be faster than in-person clinic visits.
- Urgent care and retail clinics are options if you don't have a doctor, you can't or don't want to wait to see your own doctor, or a telehealth visit can’t treat the problem.
- Virtual care from your primary provider or a telehealth service can be delivered through your smartphone, computer, or tablet.
Call 911 Now
Based on your answers, you need emergency care.
Call 911 or other emergency services now.
Sometimes people don't want to call 911. They may think that their symptoms aren't serious or that they can just get someone else to drive them. Or they might be concerned about the cost. But based on your answers, the safest and quickest way for you to get the care you need is to call 911 for medical transport to the hospital.
Make an Appointment
Based on your answers, the problem may not improve without medical care.
- Make an appointment to see your doctor in the next 1 to 2 weeks, or contact your telehealth provider.
- If appropriate, try home treatment while you are waiting for the appointment.
- If symptoms get worse or you have any concerns, call your doctor or telehealth provider. You may need care sooner.
What are your options for medical care?
Today your options for where to get your medical care are greater than ever before. You may not even have to leave your home to get the care you want and need. You can choose based on what your health problem is and what works best for you.
- Telehealth is a video call with a health care provider. It can be a convenient way to get medical advice or treatment. Some insurers provide access to telehealth that may be available 24 hours a day. Telehealth for less serious problems may cost less and be faster than in-person clinic visits.
- Urgent care and retail clinics are options if you don't have a doctor, you can't or don't want to wait to see your own doctor, or a telehealth visit can’t treat the problem.
- Virtual care from your primary provider or a telehealth service can be delivered through your smartphone, computer, or tablet.
Self-Care
Try the following tips to help relieve pain, swelling, bruising, and stuffiness when you have a minor nose injury.
- Reduce pain, swelling, and bruising.
- Use ice. Cold will reduce pain and swelling. Apply an ice or cold pack right away to prevent or have less swelling. Apply the ice or cold pack for 10 to 20 minutes. Try to do this every 1 to 2 hours for the first 3 days (when you are awake) or until the swelling goes down. Always keep a cloth between your skin and the ice pack.
- Keep your head elevated, even while you sleep. This will help reduce swelling.
- Do not take nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil or Motrin) or aspirin for the first 48 hours. Aspirin makes your blood take longer to clot, and it may cause more nose or facial bleeding. Also, do not give aspirin to children and teens. It has been linked to Reye syndrome, a rare but serious illness.
- Do not smoke. Smoking slows healing because it decreases blood supply and delays tissue repair.
- Relieve a stuffy nose, and help your sinuses drain.
- Drink plenty of fluids. Extra fluids help keep mucus thin and draining, which may help prevent blocked sinuses.
- Try a nonprescription decongestant or use saline nasal sprays or drops to relieve a stuffy nose.
- Use a cool-mist humidifier to keep the air in your home moist. Follow the directions for cleaning the machine. You may want to try using a small one in your bedroom while you sleep.
- Inhale steam from a vaporizer, or take long, steamy showers. You may also try breathing the moist air from a bowl of hot water. Put a towel over your head and the bowl to trap the moist air.
If you think you have a more serious nose injury or have a crooked nose, you may need to see a doctor.
When to call for help during self-care
Call 911 anytime you think you may need emergency care. For example, call if:
- You have trouble breathing.
- You passed out (lost consciousness).
Call a doctor if any of the following occur during self-care at home:
- New eye or vision changes.
- New signs of an infection, such as redness, warmth, swelling, pus, or a fever.
- New signs of a sinus problem, such as pain or pressure around the nose or eyes.
- Symptoms occur more often or are more severe.
Learn more
Preparing For Your Appointment
Related Information
Credits
Current as of: October 1, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: October 1, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.